Page 33 - 2016-2021-ISU
P. 33
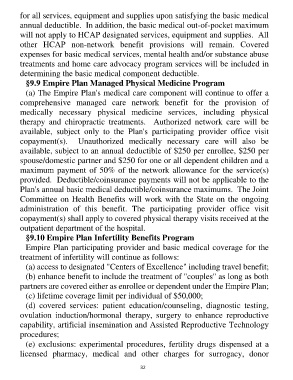
for all services, equipment and supplies upon satisfying the basic medical
annual deductible. In addition, the basic medical out-of-pocket maximum
will not apply to HCAP designated services, equipment and supplies. All
other HCAP non-network benefit provisions will remain. Covered
expenses for basic medical services, mental health and/or substance abuse
treatments and home care advocacy program services will be included in
determining the basic medical component deductible.
§9.9 Empire Plan Managed Physical Medicine Program
(a) The Empire Plan's medical care component will continue to offer a
comprehensive managed care network benefit for the provision of
medically necessary physical medicine services, including physical
therapy and chiropractic treatments. Authorized network care will be
available, subject only to the Plan's participating provider office visit
copayment(s). Unauthorized medically necessary care will also be
available, subject to an annual deductible of $250 per enrollee, $250 per
spouse/domestic partner and $250 for one or all dependent children and a
maximum payment of 50% of the network allowance for the service(s)
provided. Deductible/coinsurance payments will not be applicable to the
Plan's annual basic medical deductible/coinsurance maximums. The Joint
Committee on Health Benefits will work with the State on the ongoing
administration of this benefit. The participating provider office visit
copayment(s) shall apply to covered physical therapy visits received at the
outpatient department of the hospital.
§9.10 Empire Plan Infertility Benefits Program
Empire Plan participating provider and basic medical coverage for the
treatment of infertility will continue as follows:
(a) access to designated "Centers of Excellence" including travel benefit;
(b) enhance benefit to include the treatment of "couples" as long as both
partners are covered either as enrollee or dependent under the Empire Plan;
(c) lifetime coverage limit per individual of $50,000;
(d) covered services: patient education/counseling, diagnostic testing,
ovulation induction/hormonal therapy, surgery to enhance reproductive
capability, artificial insemination and Assisted Reproductive Technology
procedures;
(e) exclusions: experimental procedures, fertility drugs dispensed at a
licensed pharmacy, medical and other charges for surrogacy, donor
32