Page 38 - 2016-2021-OSU
P. 38
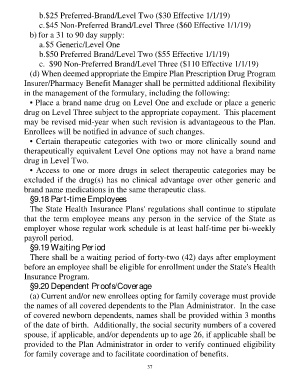
b. $25 Preferred-Brand/Level Two ($30 Effective 1/1/19)
c. $45 Non-Preferred Brand/Level Three ($60 Effective 1/1/19)
b) for a 31 to 90 day supply:
a. $5 Generic/Level One
b. $50 Preferred Brand/Level Two ($55 Effective 1/1/19)
c. $90 Non-Preferred Brand/Level Three ($110 Effective 1/1/19)
(d) When deemed appropriate the Empire Plan Prescription Drug Program
Insurer/Pharmacy Benefit Manager shall be permitted additional flexibility
in the management of the formulary, including the following:
• Place a brand name drug on Level One and exclude or place a generic
drug on Level Three subject to the appropriate copayment. This placement
may be revised mid-year when such revision is advantageous to the Plan.
Enrollees will be notified in advance of such changes.
• Certain therapeutic categories with two or more clinically sound and
therapeutically equivalent Level One options may not have a brand name
drug in Level Two.
• Access to one or more drugs in select therapeutic categories may be
excluded if the drug(s) has no clinical advantage over other generic and
brand name medications in the same therapeutic class.
§9.18 Part-time Employees
The State Health Insurance Plans' regulations shall continue to stipulate
that the term employee means any person in the service of the State as
employer whose regular work schedule is at least half-time per bi-weekly
payroll period.
§9.19 Waiting Period
There shall be a waiting period of forty-two (42) days after employment
before an employee shall be eligible for enrollment under the State's Health
Insurance Program.
§9.20 Dependent Proofs/Coverage
(a) Current and/or new enrollees opting for family coverage must provide
the names of all covered dependents to the Plan Administrator. In the case
of covered newborn dependents, names shall be provided within 3 months
of the date of birth. Additionally, the social security numbers of a covered
spouse, if applicable, and/or dependents up to age 26, if applicable shall be
provided to the Plan Administrator in order to verify continued eligibility
for family coverage and to facilitate coordination of benefits.
37